First Evidence of Microplastic Mobilization in a Human Subject – A Self-Experiment
I mobilized millions of microplastics in my blood using a simple supplement protocol. Could this be the key to clearing them from our bodies?
A few months ago, I was shocked to learn that I most likely have about a plastic spoon’s worth of plastic in my brain. You do too. Not in one piece, but spread throughout the organ, as tiny micro- and nanoparticles trapped within and between your cells.
And it isn’t just your brain. Microplastics are present nearly everywhere researchers look. They are present in your liver, your kidneys, and in your blood. And they are ubiquitous in the environment. They have infested the ocean, our soils, other animals, and even plants.
When you eat an apple, you ingest millions of microplastic particles. Drink bottled water? You are ingesting more than 100,000 particles per liter. They are entering your body through your nasal mucosa and through your lungs every day, simply by breathing.
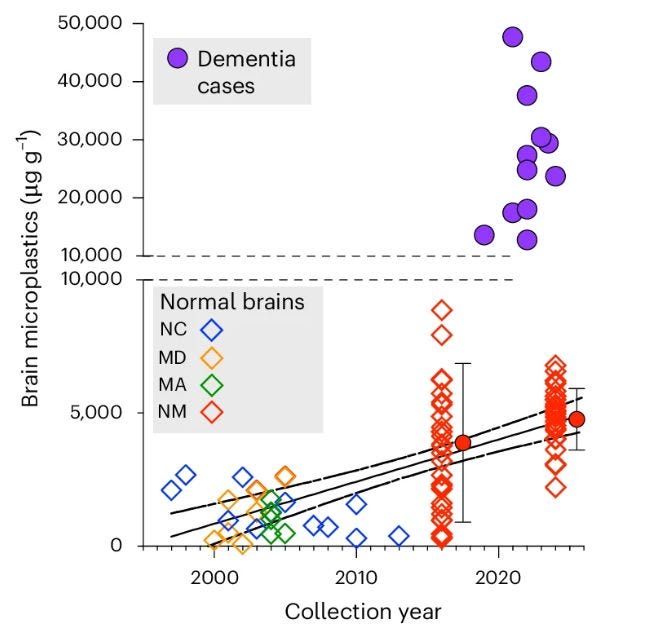
This is new information, enabled by sensitive detection methods that weren’t available just a few years ago. And we are only starting to grasp the health consequences. In animal and cell models, internalization of these particles invariably leads to cellular dysfunction and inflammation. In observational studies, microplastic burden strongly correlates with negative health outcomes – brains with dementia have more microplastics than healthy ones, and people with detectable microplastics in their arteries are more than twice as likely to have a heart attack or stroke, or to die of any cause than people without.
Once these particles enter our bodies, there is little we can do to remove them. Reducing exposure to new particles is the best we can do—at least, according to most experts. But my self-experiments suggest otherwise.
How did we get here?
These particles are the unfortunate byproducts of plastic waste. Since the polymer structure of plastic is not found in nature, nothing in nature has evolved to degrade it. This sets it apart from “biodegradable” materials, which are broken down by microorganisms that secrete specialized enzymes capable of digesting natural polymers like cellulose, lignin, and collagen.
Plastic doesn’t undergo this kind of enzymatic degradation. Instead, it is subject only to mechanical or physical weathering. Over many years, large materials are broken into smaller particles, which are themselves broken into even smaller particles, and so on. Eventually, the particles become microscopically small, at which point they are easily mobilized in the environment through things like rain and wind.
When they are ingested by plants or animals, they end up in our food supply. When you eat these plants and animals, or drink plastic-laden water, or breathe contaminated air, these microplastics end up in your body.
Most of them pass through without harm. But some small fraction are internalized through the gut or lungs and spread through the bloodstream to the rest of the body. Immune cells recognize the particles as foreign material and engulf them. They attempt to degrade the particles in their lysosomes, which would work for most natural substances, but, again, since their enzymes can’t degrade plastic, nothing happens. Instead, the microplastics sit inside the cells, causing dysfunction and inflammation or even killing the cell.
What can we do about this?
Not much, unfortunately. Thus far, reducing your exposure has been the only viable route to addressing the problem. But with microplastics present in nearly every food source and in the very air we breathe, exposure reduction will only go so far.
Yes, eliminating the worst offenders is logical and likely helpful. Switch from bottled water to tap or home purified water. Stop microwaving foods in plastic containers. Use a refillable steel or ceramic travel mug for your coffee or tea (the plastic liner in those paper cups releases thousands of microplastics). Invest in a good air purifier for your home.
But don’t fool yourself. Even with these changes, you’ll still be ingesting microplastics. There is no way around it.
We need smart solutions, and I suspect that we will soon see a robust industry take shape with the stated goal of addressing the microplastics problem. Engineered enzymes or bacteria could break the polymers down in the gut, before they enter our circulation. Binding agents could block absorption. Better yet, engineered, plastic-degrading bacteria could be introduced into agricultural soils, reducing plastic levels in our food supply. We might even see drugs that can break the polymers down once absorbed systemically.
The bad news is that advanced solutions won’t be ready any time soon. We are at least five to ten years away from a breakthrough, and even then, nothing is guaranteed. The brightest minds in the field agree that reducing exposure is the best that we can do today.
But, what if there were a simple protocol that could leverage existing tools to eliminate plastics that are already present in our cells? What if cells could be “tricked” into releasing microplastics back into the blood, where they could be transported to the liver for biliary excretion, or even actively removed with plasma exchange?
A Novel Approach for Microplastics Elimination
First, some necessary background.
When microplastics enter systemic circulation they can meet a number of fates. The smallest class of particles, less than about 10 microns (μm) in diameter, can penetrate deeply into tissues, taking up residence either between or within cells. This is where they presumably cause the most problems, interrupting cell and organ function, driving inflammation, and accelerating aging-related processes.
Immune cells like macrophages can also engulf these small particles quite efficiently through a process called phagocytosis, the same one that they use to clear cellular debris or pathogens. Other cells use a similar process called endocytosis. Once engulfed, the materials are sent to the lysosome, where the cells try to break them down with acids and enzymes.
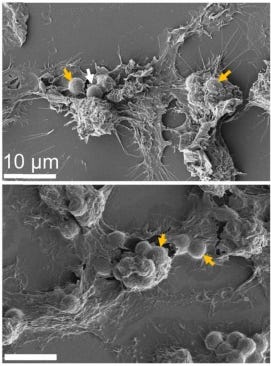
Even small particles like this (<10 μm, yellow arrows) take up a massive volume within immune cells like macrophages:
Unlike natural substrates, cells aren’t able to digest the microplastics. Instead, the particles remain within the cells, driving an aberrant inflammatory state. The lysosomes, now full of plastic, can’t perform their normal function of turning over wastes. The cells stop doing their jobs and instead release cytokines that can damage neighboring cells, causing local tissue damage and irritation.
We don’t know the exact consequences of this process yet, but we know that disrupting lysosomal function more broadly is terrible for health, even driving severe lysosomal storage disorders that result in disability and death.
Fortunately, some of these small particles are also cleared by the kidney or liver and eliminated via urine or feces (in bile), respectively, a far more desirable fate.
Larger particles, in the 10-70 μm range or even greater, aren’t transported deeply into tissues with the same efficiency, although they can still be cleared via urine, a somewhat surprising finding. Some may also be cleared through bile, but just as with smaller particles, immune cells recognize many of these particles and try to engulf them. For some of the smaller particles in this range, the immune cells succeed, although the engulfed particle is almost the size of the cell itself—you can imagine the cellular damage that this causes. For the larger particles, the cells need another strategy.
When macrophages encounter very large debris, multiple cells can actually fuse together, forming a giant cell that can then engulf the target. These cells can comfortably engulf plastic debris at least up to 40 μm, but still can’t digest it once in the lysosome. When they fill up with plastics, they will have all of the same problems as with smaller cells and particles. They will become dysfunctional inflammation machines.
For a cell biologist, this is scary stuff. But, understanding this biology can help us formulate a strategy for clearance.
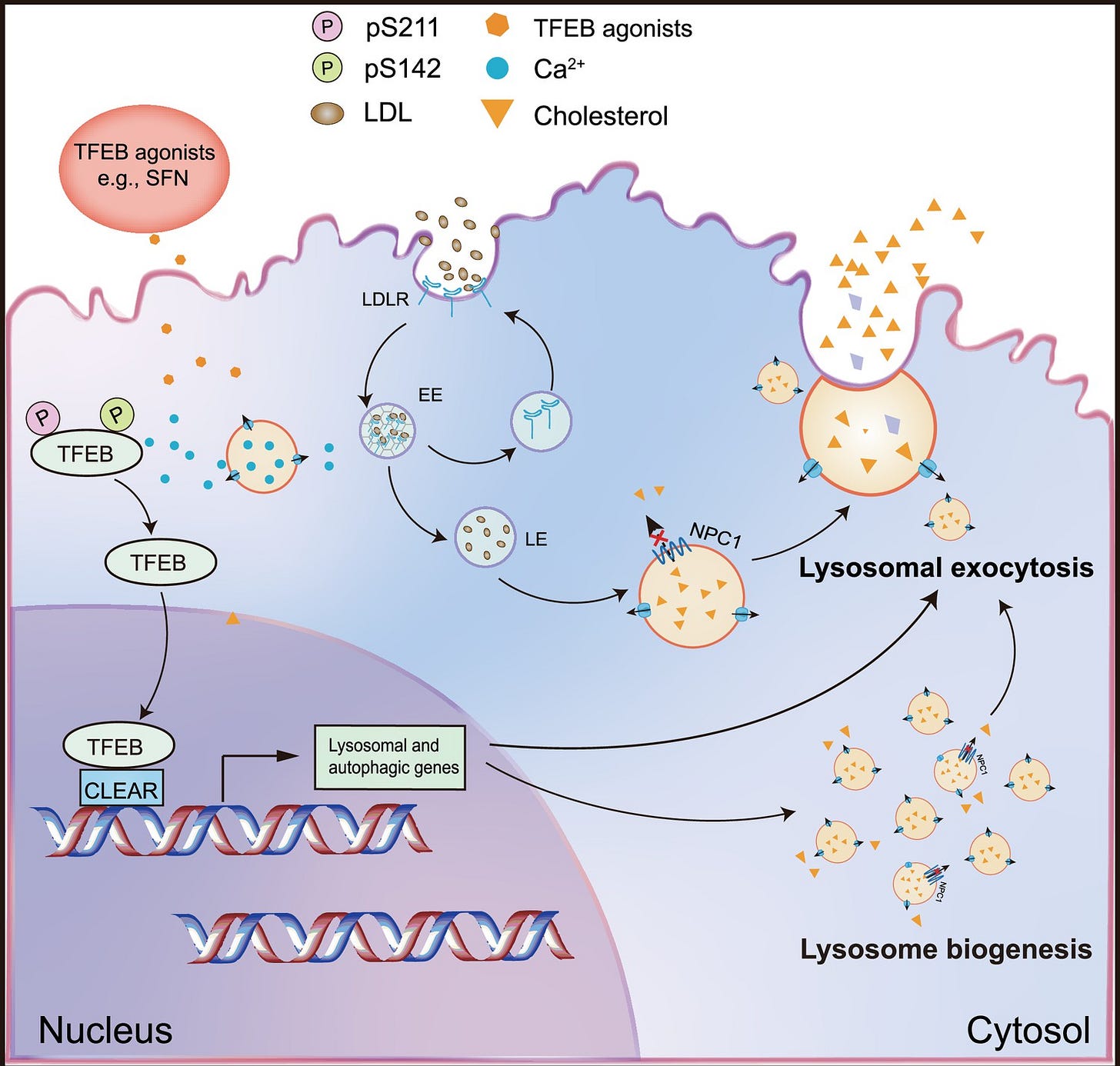
Thankfully, digestion isn’t the only way for materials to leave the lysosome. Cells have evolved a coordinated lysosomal stress response that can push lysosomes to dump their contents outside of the cell (a process called exocytosis), where particles have another chance to be eliminated. And we can activate this pathway with drugs.
Sulforaphane Boosts Lysosomal Exocytosis
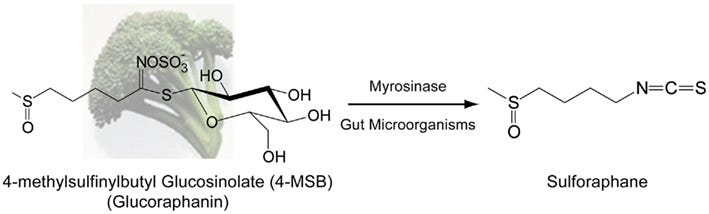
Sulforaphane is an incredibly interesting compound. Derived from broccoli, it is, at the most basic level, a potent cell stressor. It is highly reactive, permanently attaching itself to proteins within cells. Left unchecked, this could disrupt all sorts of cellular processes. But, as you might imagine, evolution has found ways to protect against this.
Several proteins are exquisitely sensitive to stress from compounds like sulforaphane. These proteins essentially act as oxidative stress sensors, and when they are activated, they kick off a coordinated stress response, stimulating the cell to make more antioxidant proteins, more lysosomes, and more machinery for autophagy (the process that delivers many materials to the lysosome for degradation). This also causes cells to push lysosomes toward exocytosis, dumping their contents into the extracellular space for clearance. This can help to remove the offending toxin, clear proteins damaged by it, and restore a healthy cellular environment.
The antioxidant side of this stress response is driven by a protein called NRF2, and NRF2 activation is what you typically hear about with sulforaphane—hence the use as a booster of antioxidant and detox pathways. The lysosomal side is driven by a protein called TFEB; activation of this pathway by sulforaphane is a newer finding and is only starting to be widely appreciated. Other drugs can also activate TFEB, but sulforaphane seems to do it quite potently and effectively. It is also widely available as a highly pure supplement, and has a well-documented track record of safety in humans, making it an appealing candidate for therapeutic intervention.
A few weeks ago, a groundbreaking study reported the use of sulforaphane to treat a mouse model of Niemann-Pick disease Type C, a rare pediatric disease caused by the accumulation of cholesterol and fats within the lysosome. Normally, this accumulation leads to the widespread death and dysfunction of neurons. But when treated with sulforaphane, the mice dumped the excess materials from their lysosomes into the extracellular space, where it could be cleared away. This spared neurons from death and improved the health of the mice.
Sounds useful, right?
Testing Sulforaphane as a Microplastics Mobilizer
Neimann-Pick disease Type C is a severe example of lysosomal dysfunction, but the same strategies that work here could potentially work for any condition where lysosomal exocytosis is desired. And that includes microplastics accumulation.
A typical individual has a steady stream of microplastics moving both into and out of their body every day. The problematic particles are the ones that get stuck. It might therefore be therapeutically useful to encourage cells to release microplastics from their lysosomes so that they have another chance for clearance. Once relieved of this inflammatory stimulus, the cells could then go back to doing their jobs and stop generating harmful inflammation throughout our bodies.
Sulforaphane is well-poised to encourage exactly this. By activating TFEB (and another target called MCOLN1), sulforaphane could stimulate plastic-filled cells to exocytose their lysosomes, releasing the microplastics back into circulation.
This is biologically plausible, has therapeutic potential, and is easily measured with a new test from Bryan Johnson’s Blueprint. In other words, it has all the makings of an exciting self-experiment. So, I went for it.
The Sulforaphane Test Protocol
To minimize interference from dietary sources, I standardized my diet for two days before the experiment and throughout its duration. I also standardized things like exercise, sleep and wake time, and water consumption. Each morning, for four days, after a 12 hour fast, I took a small sample of blood from a finger prick using only plastic-free materials. I measured microplastics in the blood samples with the CLIA-certified Blueprint test.
Day 0 served as my baseline, reflecting my typical blood microplastics level without intervention. At day 0 +12 hours, I took 100 mg of stabilized sulforaphane (Mara-Labs BrocElite Plus) with a high-fat meal to ensure optimal absorption. This is higher than the labeled dose or the doses usually used for general health promotion, but I wanted the best chances of generating a strong, measurable signal. 100 mg is similar to the highest dose tested in clinical studies, which gave me confidence in safety. If someone were to try this therapeutically, I would recommend sticking to the manufacturer’s recommendation of 10 mg, which still has a measurable biological effect.
The first post-dose measurement was on day 1, 12 hours after dosing, prior to any expected effect from TFEB activation. Since TFEB works by activating gene transcription, it takes some time to transcribe RNA from DNA and to translate the mRNA into protein. A peak lysosomal exocytosis response would therefore be expected somewhere in the 24-48 hour range or on day 2. The day 3 reading would be expected to reflect either a lingering exocytosis response or a return to baseline levels.
My (Surprising) Results
My baseline reading wasn’t anything special. I had 39 particles in my 0.1 mL blood sample, more than 78% of the population and less than 15% of the population. A little over half of them (22 particles) were smaller than 10 μm, while the remainder were 10-30 μm. I didn’t have any of the largest sized particles (30 - 70 μm) in my blood; if any were in my body, they were likely trapped in the lysosomes of giant cells within my tissues.
Nothing really changed for any of the particle classes on day 1, just some small fluctuations likely reflecting day-to-day variability. This is exactly as I expected, since 12 hours really isn’t long enough for sulforaphane to activate TFEB.
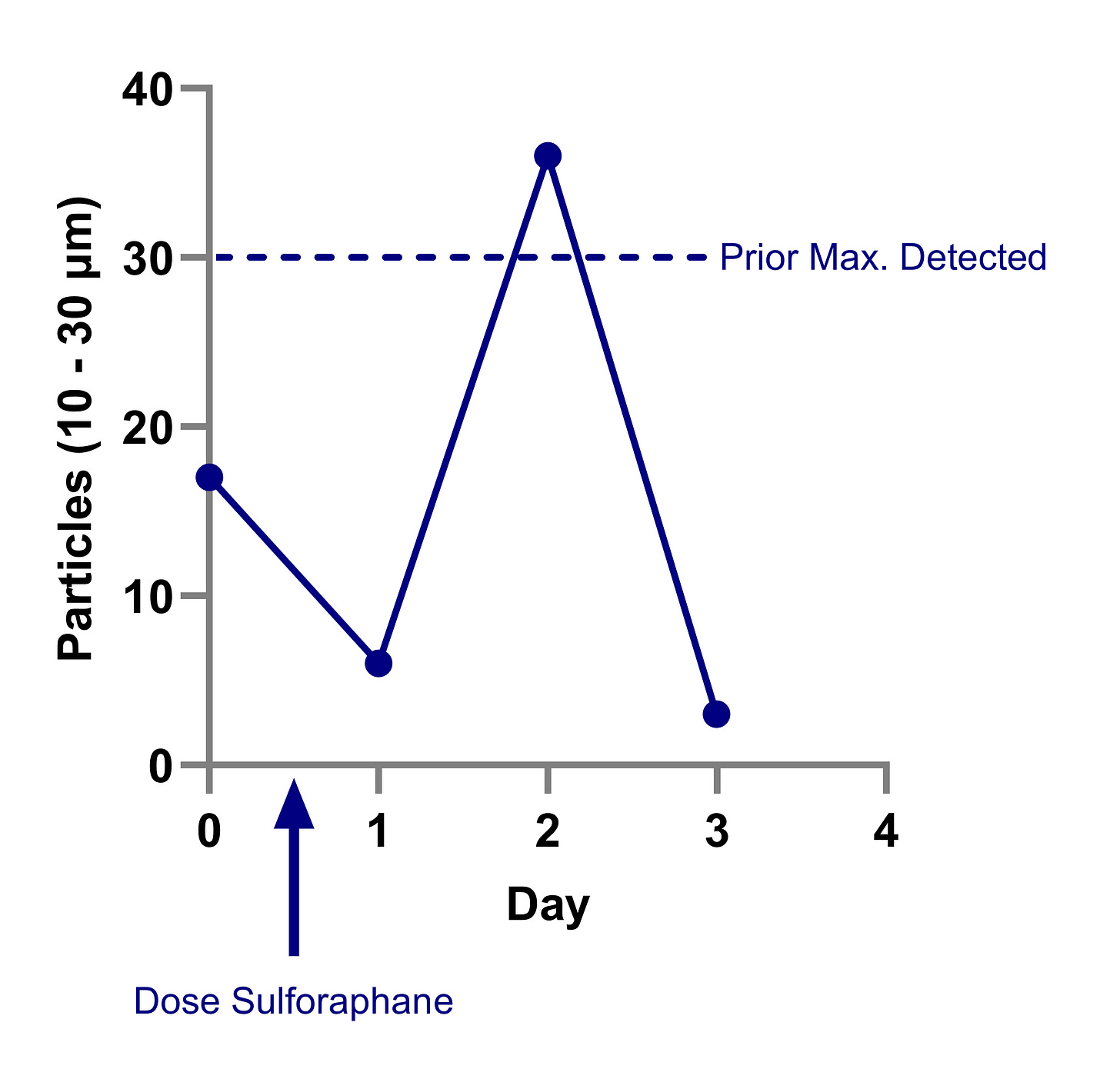
But on day 2, things got incredibly interesting. For the larger particle classes, I didn’t just see the small bump that I expected—I saw an absolutely massive spike. Particles in the 10 - 30 μm range more than doubled from 17 to 36. According to the test report, this was well above the maximum levels previously detected in 2,100 previously measured users. In other words, it was literally off the charts.
The same was true for the largest particles in the 30-70 μm range, which spiked from 0 to 7. This was nearly twice the maximum previously detected by the testing company.
In other words, the sulforaphane protocol didn’t just increase my blood microplastics above baseline, it resulted in the highest levels of large particles ever recorded by the testing company. That is about the cleanest result I could have hoped for in an n-of-1 study like this, and gives me great confidence that the signal is the result of sulforaphane causing cells to dump microplastics into circulation, rather than a random environmental exposure or day-to-day variability.
Remember, all of these numbers reflect the number of particles present in a 0.1 mL sample of blood. Since the human body contains about 5 L of blood, total levels are much higher. For example, seeing the 30-70 μm particles jumping to 7 in the day 2 sample means that approximately 350,000 of these particles were mobilized throughout the body. For particles in the 10 - 30 μm range, the spike of 36 in the sample equates to about 1.8 million particles body-wide.
The Fate of Mobilized Microplastics
So, sulforaphane mobilized microplastics in the 10-70 μm range, but where did they go? This is where my experimental data ends and pure speculation begins.
Some of them were probably taken up by new immune cells, or redistributed to tissues, where they became stuck again. Some may have been excreted in the urine or in bile, something I would have loved to have measured but which was not possible without a test that has been developed for those biofluids. Without those data, I can’t say with any certainty that mobilization resulted in actual clearance.
One interesting wrinkle: microplastics in the <10 μm range didn’t really move outside of the typical variability observed by the testing company. Is this because they are more amenable to clearance and don’t accumulate in the blood the way that large particles do? Perhaps. Or maybe they are more readily taken up into new immune cells. Or, the temporal pattern could be different here, and there was a transient spike that wasn’t captured on any of the daily readings. Measurements of elimination would have been really helpful here, but those will have to wait for a new set of experiments pending availability of new tools like urine tests.
Still, this could be the beginning of an actual strategy.
Imagine this. A health-focused individual has reduced their microplastics exposure as much as reasonably possible, but they are still showing substantial levels on blood tests, just like I was.
They take sulforaphane. 36 hours later, stubborn particles trapped in their cells have been mobilized into the blood. They take advantage of this window by going to their local longevity clinic for therapeutic plasma exchange (TPE, which has potent anti-aging benefits on its own). This removes millions of liberated particles, dramatically decreasing their microplastics load.
To stay on top of their ever-present exposure, they repeat this on an annual basis, keeping their lysosomes and immune cells in a more youthful, less inflamed state.
This isn’t far-fetched in the slightest. And TPE might even be overkill; a good portion of the mobilized microplastics may be eliminated on their own, or could be encouraged to do so with other smart drug protocols used alongside sulforaphane.
This experiment is only the beginning. To my knowledge, this is the first evidence of drug-induced microplastics mobilization in a human subject. But this is by no means the best strategy that will be developed.
While many questions remain—particularly how effectively these mobilized particles are cleared from the body—the potential implications are enormous. This simple, accessible approach could form the foundation of practical, proactive strategies to reduce microplastic burden, limit chronic inflammation, and support long-term health.
If you’ve tried anything to reduce your microplastics burden, or if you have ideas, drop a note in the comments. I’d love to hear what you’re thinking.











Broccoli sprouts are the most concentrated source of glucoraphanin which is converted to sulforaphane when sprouts are eaten. The inclusion of broccoli sprouts in your diet could have a major impact on microplastic reduction if your hypothesis is correct. They are delicious and a versatile ingredient. See www.wildaboutsprouts.com for more information.
Perhaps a rather unethical, but just hypothetical question, would it work just as well to donate the plasma as do the therapeutic plasma exchange? Not everyone can afford $10,000 to get rid of their microplastics!